What Is Medicare Open Enrollment
Medicare open enrollment is a designated window of time each year when individuals can make changes to their Medicare coverage.
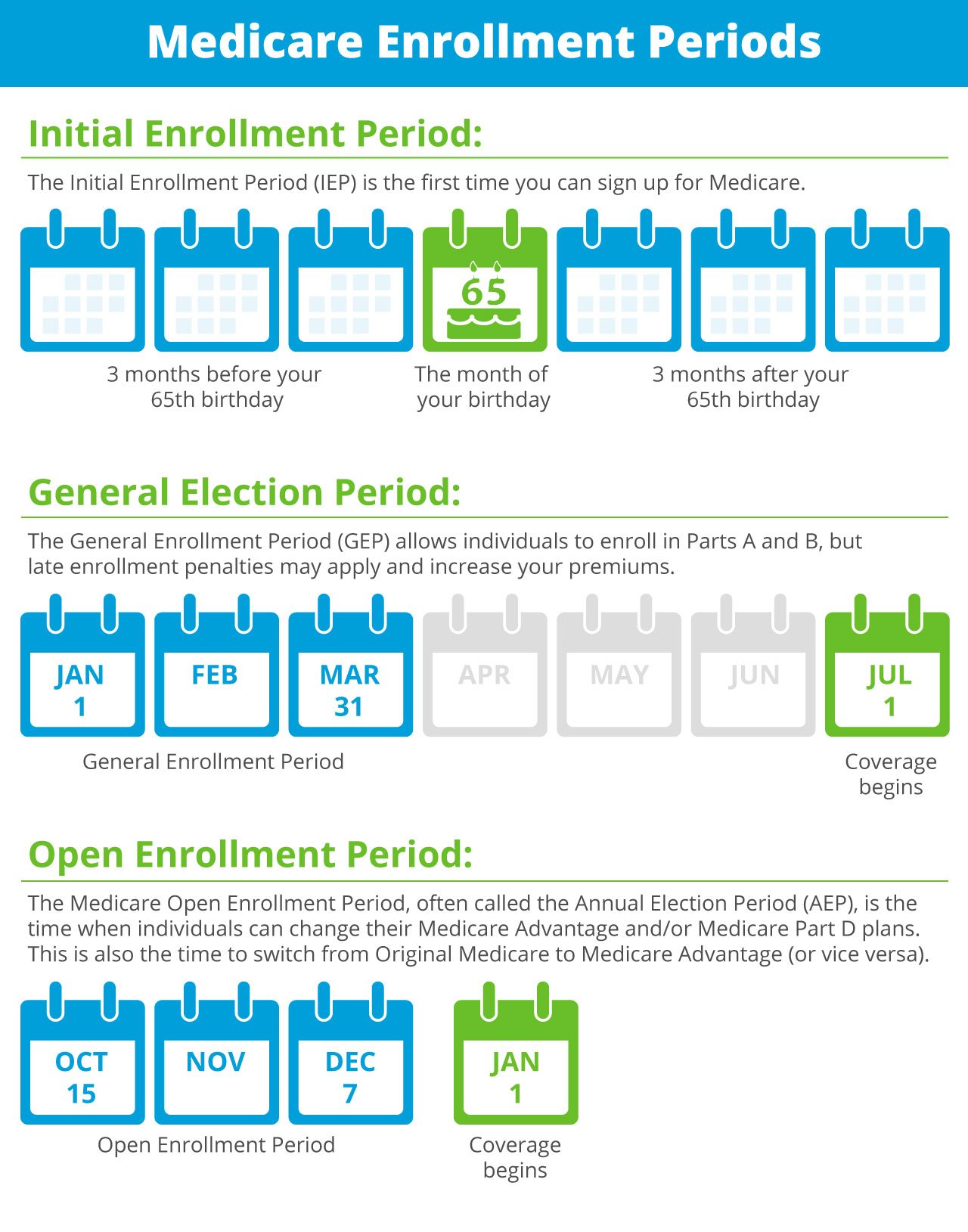
Open enrollment is primarily for people who already have Medicare. New applicants should sign up during their initial enrollment period, which starts three months before they turn 65 and ends three months after the month they turn 65. If they miss their initial enrollment period, they can sign up during open enrollment.
The fall open enrollment period for Medicare begins Oct. 15 and runs through Dec. 7 in 2021. This enrollment period is open to people who are covered by:
- Medicare Part A
- Medicare Part B
- Original Medicare
A separate Medicare open enrollment period applies to people who are covered by a Medicare Advantage plan . The open enrollment period for Medicare Advantage plans runs from Jan. 1 to March 31 each year.
Changing Medicare Advantage Plans Or Part D Plans Outside Of Open Enrollment
Many Medicare beneficiaries enroll in a Medicare Advantage plan or a Medicare Part D prescription drug plan during the Medicare Open Enrollment Period for Medicare Advantage and prescription drug plans.
During this period , you can make a number of coverage changes:
- You can change from one Medicare Advantage plan to another, whether or not either plan includes prescription drug coverage.
- You can disenroll from your Medicare Advantage plan and switch back to Original Medicare .
- If you switch back to Original Medicare during this period, you can join a Medicare Part D prescription drug plan.
If you dont enroll in a Medicare plan during this annual period, you may qualify for a Special Enrollment Period.
There are many ways to qualify for a Medicare Advantage Special Enrollment Period or a Medicare Part D Special Enrollment Period.
Some of the situations that may qualify you for one of these types of Special Enrollment Periods include:
The above list does not necessarily include every and all qualifications for a Special Enrollment Period.
What Types Of Enrollment Periods Does Medicare Use
Medicare’s standard enrollment periods are:
Special Enrollment Periods are available to people experiencing what Medicare calls special circumstances, such as losing your employer coverage or moving. The full list is available on Medicare.gov here.
The Medicare Part B Special Enrollment Period is available to those who delay signing up for Part B because they have coverage through an employer . Once that coverage ends, they qualify for an SEP that lasts for eight months. It begins either the day coverage ends or the day employment ends whichever comes first.
Please note that, to qualify for the Part B SEP, you must have been actively employed. Health insurance through a retirement plan or COBRA does not qualify as you are not “actively” employed. The same is true if the insurance is through a spouse’s employment. Once you or your spouse is no longer actively employed, the Part B Special Enrollment Period begins. Full details are available from the Social Security Administration here.
Don’t Miss: My Period Is 2 Days Late Should I Be Worried
Special Election Period For Medicare Advantage And Medicare Prescription Drug Plans
The Special Election Period , also called a Special Enrollment Period, for Medicare Advantage and prescription drug plans is generally somewhat different from the Original Medicare SEP.
Typically, the Medicare Advantage/prescription drug SEP applies to those who have lost their coverage. For example, if your plan stopped accepting Medicare or moved out of your area, or if you moved out of the plans service area, you might be eligible.
Another situation where you might qualify for a Medicare Advantage/prescription drug SEP is if your area is hit with a natural disaster. For this SEP, there are several restrictions you should be aware of. All of these must be true for you:
- The Federal Emergency Management Agency declared an emergency or major disaster in your county.
- You lived in the affected county when FEMA declared the emergency or major disaster.
- You had a valid election period going when FEMA declared the emergency or major disaster.
- You hadnt yetchanged your coverage when the emergency or major disaster was declared.
- The valid SEP for your situation hasnt expired.
For more information, read about FEMA-related Special Enrollment Periods.
Enter your zip code on this page to start comparing plans with no obligation.
Medicare Special Enrollment Period For Disabled Tricare Beneficiaries
TRICARE is health insurance for retired and active-duty service members and their families. If youre a retired service member, you must enroll in Part B to stay eligible for TRICARE benefits. However, TRICARE beneficiaries who qualify for Medicare based on disability, Lou Gehrigs disease or end stage renal disease may qualify for a Medicare Special Enrollment Period if they didnt sign up for Part B during their Initial Enrollment Period. This 12-month SEP starts on:
- The last day of the persons Initial Enrollment Period, or
- The month that the person is notified of Part A enrollment
This Medicare Special Enrollment Period can only be used one time during the TRICARE beneficiarys lifetime.
Also Check: Periodic Table With Real Elements Inside
Who Is Eligible For A Medicare Special Enrollment Period
In order to qualify for the Original Medicare Special Enrollment Period, you must have been in your Initial Enrollment Period , General Enrollment Period or another Special Enrollment Period between March 17 and June 17 and did not submit an enrollment request to the Social Security Administration.
In other words, if you were eligible to enroll in Medicare Part A or Part B for the first time at any point between March 17 and June 17 but did not do so, you may be eligible for this Special Enrollment Period.
In order to qualify for the Special Enrollment Period for Medicare Advantage, Medicare Part D and Medicare/Medicaid plans, you must have had a valid enrollment period between March 17 and June 30 and did not make any changes to your coverage at this time.
Valid enrollment periods include your IEP, another Special Enrollment Period or the Medicare Advantage Annual Enrollment Period that occurs each fall.
| For either enrollment period, it is not required to show any proof that you failed to take enrollment action due to COVID-19. Qualification is based on the above criteria. |
Signing Up For Premium
You can sign up for Part A any time after you turn 65. Your Part A coverage starts 6 months back from when you sign up or when you apply for benefits from Social Security . Coverage cant start earlier than the month you turned 65.
After your Initial Enrollment Period ends, you can only sign up for Part B and Premium-Part A during one of the other enrollment periods.
Don’t Miss: Medicare Open Enrollment Period 2020 Extended
Enrollment In Medicaid A Medicare Savings Program Or Extra Help
If you are enrolled in Medicaid, a Medicare Savings Program or Extra Help, you may join, disenroll from or switch Medicare Advantage plans beginning the month you first become eligible for Medicaid or MSP and may continue to switch plans once a month thereafter.
If you lose Medicaid, MSP or Extra Help benefits, you will be granted a one-time opportunity to make changes in your Medicare Advantage enrollment.
Medicare Special Enrollment Period For International Volunteers
Individuals volunteering in a foreign country may be able to enroll in Part A and/or Part B with a Medicare Special Enrollment Period when they return to the United States. To qualify for a Medicare Special Enrollment Period, you must:
- Have volunteered for at least 12 months outside of the United States
- Have volunteered for a tax-exempt program
- Have had other health coverage for the duration that you served overseas
Also Check: Dental Coverage With No Waiting Period
How To Enroll In And Change Medicare Plans
Once youve signed up for Medicare, youll have several options for changing certain aspects of your health coverage. Heres an outline:
During the annual open enrollment window , you can make several changes, none of which require medical underwriting:
- Change your Medicare Advantage plan to Original Medicare or vice versa.
- Switch from one Medicare Advantage plan to a different one.
- Change from one Medicare Part D prescription plan to another. It is strongly advised that all recipients use Medicares program finder tool each year to compare available Part D plans, rather than simply allowing an existing drug plan to auto-renew.
- Sign up for a Medicare Part D plan.
- You can cancel your Part D coverage entirely.
During the Medicare Advantage open enrollment period, US citizens who already registered in Medicare Advantage plan can:
- Change to Original Medicare plan
- Change to a new Medicare Advantage plan.
- Only one plan alteration is allowed .
During the five-star registration period , persons who reside in a state with a five-star Medicare Advantage plan or Medicare Part D can switch to that program.
During the first year of Medicare Advantage enrollment, a person can change to an Original Medicare plan and a Part D coverage. They also have full access to a Medigap plan, with some exceptions.
A person registered in Original Medicare can apply for a new Medigap plan at any time of the year.
Disenrollment From Your First Medicare Advantage Plan
If you enrolled in a Medicare Advantage plan when you first became eligible for Medicare, you have 12 months to disenroll from the plan and transition back to Original Medicare.
If you dropped a Medicare Supplement Insurance plan to enroll in a Medicare Advantage plan but wish to revert back again, you have 12 months to do so .
Read Also: Can The First Depo Shot Stop Your Period
If You Miss Medicare Open Enrollment
If you miss the Medicare open enrollment period you generally can’t make any changes to your coverage until the next one rolls around. There are, however, some exceptions. Special Enrollment Periods allow you to update your coverage under certain conditions. You may qualify if you:
- Relocate to an area that isn’t in your current plan’s service area
- Relocate to an area that offers new coverage options for your current plan
- Move into or out of a skilled nursing care facility
- Are released from jail
- Move back to the U.S. after living outside the country
- Leave coverage from an employer or COBRA coverage
- Dropped your coverage in a Program of All-Inclusive Care for the Elderly
- Were but no longer are longer eligible for Medicaid
- Are enrolled in a Medicare Advantage plan or Part D plan that isn’t renewed
- Are eligible for both Medicaid and Medicare
- Qualify for the Extra Help program to pay for Medicare Part prescription drug coverage
Those are just some of the situations in which you may be eligible to change your Medicare plan outside of the open enrollment period. You can learn more about special enrollment periods on the Medicare website.
What Events Trigger A Special Enrollment Period For Medicare

Medicare is the federal health insurance program designed for people who are 65 years of age or older. It also provides coverage for some younger people with disabilities and people who have end-stage renal disease . When you become eligible for Medicare, you need to decide when to enroll.
You can enroll during the initial enrollment period, which begins near your 65th birthday and lasts for seven months. You can also enroll during the general enrollment period , but you may face late enrollment penalties. If youre already enrolled, you can make changes to your coverage during designated open enrollment periods each year, depending on the type of coverage you have.
But if you need to add or change your coverage outside of these times, you must qualify for a special enrollment period . Several different events can create these enrollment opportunities. Below, youll find which circumstances make you eligible for a special enrollment period, and what Medicare programs you can enroll in.
Read Also: Severe Lower Back And Hip Pain During Period
Enrolling In A Medicare Supplement
During your initial Medigap enrollment period you cant be denied Medigap coverage or be charged more for the coverage because of your medical history.
But after that window ends, Medigap insurers in most states can use medical underwriting to determine your premiums and eligibility for coverage.
If youre under 65 and eligible for Medicare because of a disability, there are 33 states that provide some sort of guaranteed issue period during which you can purchase a Medigap plan. But in the majority of those states, the carriers can charge additional premiums for people under 65. You can click on a state on this map to see how Medigap plans are regulated in the state.
To find out about Medigap policies in your state, contact your State Department of Insurance or your State Health Insurance Assistance Program, or call 1-855-593-5633 to speak with one of our partners, who can help you find a plan in your area.
Special Enrollment Period Related To Covid Pandemic
The COVID-19 pandemic was uncharted territory for the United States, but its an excellent example of an exceptional circumstance that can trigger a special enrollment period. There are 28 million Americans who have no health insurance coverage, which immediately presented an obstacle to the nations ability to fight the virus.
The COVID SEP ended in most states. The American Rescue Plan is still making premiums more affordable.
To ensure that as many people as possible would be able to have coverage as the nation faced this crisis, most of the state-run exchanges announced special enrollment periods in 2020, under which uninsured residents could select a plan, even if they didnt have a qualifying event.
Under the Trump administration, HealthCare.gov did not open a COVID-related special enrollment period in 2020, although they did modify the loss-of-coverage special enrollment period requirements to allow people to use it if they had lost their health coverage at any point back as far as January 1, 2020.
But soon after taking office, the Biden administration created a special enrollment period in the 36 states that usedHealthCare.gov for 2021 coverage, giving uninsured Americans another opportunity to enroll in coverage, and providing $50 million in funding to publicize the enrollment period and make sure people know about it. The new COVID-related special enrollment period began February 15 and ended August 15, 2021.
Don’t Miss: How Long Does A First Period Last
Everything You Need To Know About This Year’s Enrollment Dates Coverage Costs Eligibility Details And Opportunities To Change Coverage
During the annual Medicare open enrollment, Medicare plan enrollees can reevaluate their coverage whether its Original Medicare with supplemental drug coverage, or Medicare Advantage and make changes if they want to do so. | Image: rocketclips / stock.adobe.com
Medicare open enrollment for 2022 coverage starts on October 15, 2021, and continues through December 7. Learn how you can change your Medicare coverage outside of the fall open enrollment period.
