Can Chlamydia And Other Stis Make You Miss Your Period
Hopefully, the information we presented here has helped you understand STIs, symptoms, and how they can impact your period. To summarize, STIs usually wont make you miss your period, but it is more likely if an untreated STI has progressed to PID. In addition to missed periods, PID can also cause spotting between periods.
Genital And Reproductive Health
Amenorrhea
Amenorrhea is the medical term referring to the state of a woman who has missed at least three periods. The name of this disorder comes from Greek, in which a means without and menorrhea means menstrual flow. It is easy to write-off missed periods as a convenience, but amenorrhea indicates your body has a problem that is preventing it from functioning normally. Athletes participating in physically demanding sports often have low estrogen levels, no matter how well balanced their diets are. Low levels of this hormone promote bone density loss, and by the time these athletes lose their period, their bones have suffered significantly. Amenorrhea can have a negative impact on reproductive, endocrine, and muscular-skeletal systems, so you should see a doctor if you go longer than 12 weeks without a period and need help to start menstruating again. Starting or ending contraception disrupts the bodys normal hormone levels, and it may take up to six months for your period to return to normal. Pregnancy is the most common reason women stop menstruating, but if youre definitely not pregnant, here are some possible causes of amenorrhea:
- low body weight
- strenuous exercise
Endometriosis
Importance of Folic Acid for Women
Gynecological check-up
- vaginal pain, burning, or itching
- vaginal sores
- severe menstrual cramps
Ovarian Cysts
Pelvic Inflammatory Disease
Premenstrual Syndrome
If these changes dont improve symptoms, you may consider medication. Medicine that may help:
Are There Any Over The Counter Treatments For Chlamydia
Treatment, however, does not prevent infections in the future, and reinfection is common. 1 There are both recommended and alternative antibiotic regimens, with specific recommendations for women who are or may be pregnant. Over-the-counter therapies are not effective against chlamydia and should not be used.
Recommended Reading: Period Blood Stains On Sheets
Home Remedies For Chlamydia Symptoms
You may still experience painful or uncomfortable symptoms while youre taking chlamydia antibiotics.
Here are some home remedies for reducing your pain and other symptoms while youre waiting for the antibiotics to work:
- pain medications, such as ibuprofen to reduce pain
- cold pack to help limit swelling and inflammation
- goldenseal to reduce inflammation and potentially make symptoms less severe
- echinacea to bolster your immune system against the infection and reduce your symptoms
- turmeric containing an ingredient called curcumin to reduce inflammation and make symptoms less severe
No studies support the effectiveness of these supplements specifically for chlamydia, so take them with caution.
And theres no substitute for antibiotics when treating chlamydia. Only try these remedies if youre already taking antibiotics or if you plan to go to the doctor.
Can Chlamydia Be Stopped Chlamydia Test Results How Long

The only certain method to avoid chlamydia is to not have vaginal, anal, or foreplay.
Right usage of latex prophylactics significantly reduces however does not get rid of, the threat of catching or spreading out chlamydia. If your or your partner is allergic to latex, you can use polyurethane prophylactics.
You May Like: How Soon Can I Get Tested For Chlamydia
Don’t Miss: 90 Day Probationary Period Form
How Is An Iud Inserted Is It Painful
In the insertion process, the cervix is opened and the IUD is placed into the uterus. While the insertion process can be slightly painful, the procedure generally takes just a few minutes. You may experience cramping for about 24 to 48 hours after the procedure as this is a common response among women after an IUD is inserted.
Urogenital Infection In Men
In men, chlamydial infection of the lower genital tract causes urethritis and, on occasion, epididymitis. Urethritis is secondary to C. trachomatis infection in approximately 15 to 55 percent of men, although the prevalence is lower among older men.2 Symptoms, if present, include a mild to moderate, clear to white urethral discharge. This is best observed in the morning, before the patient voids. To observe the discharge, the penis may need to be milked by applying pressure from the base of the penis to the glans.
The diagnosis of nongonococcal urethritis can be confirmed by the presence of a mucopurulent discharge from the penis, a Gram stain of the discharge with more than five white blood cells per oil-immersion field, and no intracellular gram-negative diplococci.2 A positive result on a leukocyte esterase test of first-void urine or a microscopic examination of first-void urine showing 10 or more white blood cells per high-powered field also confirms the diagnosis of urethritis.
For diagnosis of C. trachomatis infection in men with suspected urethritis, the nucleic acid amplification technique to detect chlamydial and gonococcal infections is best .4 Empiric treatment should be considered for patients who are at high risk of being lost to follow-up.
Read Also: I Had Chlamydia And Got Treated
Read Also: Brown Stuff Instead Of Period
How Can I Treat Vaginal Bleeding Caused By A Sexually Transmitted Infection
If your doctor has diagnosed that your bleeding is because of a sexually transmitted infection your partner also needs to be treated otherwise you will continue to reinfect each other. STIs can also cause unusual or increased vaginal discharge which will also go away after the infection has been treated. If the infection is thrush , your partner may not need treatment as just treating you is enough.
Who Should Be Tested For Chlamydia
Any sexually active person can be infected with chlamydia. Anyone with genital symptoms such as discharge, burning during urination, unusual sores, or rash should refrain from having sex until they are able to see a health care provider about their symptoms.
Also, anyone with an oral, anal, or vaginal sex partner who has been recently diagnosed with an STD should see a health care provider for evaluation.
Because chlamydia is usually asymptomatic, screening is necessary to identify most infections. Screening programs have been demonstrated to reduce rates of adverse sequelae in women.31,41 CDC recommends yearly chlamydia screening of all sexually active women younger than 25, as well as older women with risk factors such as new or multiple partners, or a sex partner who has a sexually transmitted infection.40 Rectal chlamydia testing can be considered for females based on sexual behaviors and exposure. 40 Pregnant women under 25 or older pregnant women at increased risk for chlamydia should be screened during their first prenatal visit and again during their third trimester.40 Women diagnosed with chlamydial infection should be retested approximately 3 months after treatment.40 Any woman who is sexually active should discuss her risk factors with a health care provider who can then determine if more frequent screening is necessary.
Also Check: New Hire 90 Day-probationary Period Template
What Is Pelvic Inflammatory Disease
Pelvic inflammatory disease is one potentially grave consequence of undiagnosed and untreated STIs. The answer to the Could an STD stop your period? question changes for women with PID. This severe condition definitely can cause irregular or excessively heavy periods, as well as spotting between periods.
So what is pelvic inflammatory disease? PID can occur when a pathogen, usually but not always a sexually transmitted bacteria like chlamydia or gonorrhea, spreads across the female reproductive tract, including the vagina, uterus, fallopian tubes, and pelvis.
Health care providers often have difficulty diagnosing PID because of its inconsistent, nonspecific, and sometimes nonexistent symptoms. PID can occur in the form of:
- Acute PID. The acute form of PID may manifest in high fever, severe lower abdominal pain, fainting, or vomiting. If youre experiencing these symptoms, go to the ER right away.
- Chronic PID. Chronic PID usually involves prolonged but vague complaints such as pelvic pain during intercourse, urinary problems, irregular menstrual bleeding, heavier periods with painful cramping, spotting between cycles, and abnormal vaginal discharge.
- Silent PID. In many cases, PID may cause silent but devastating damage to a womans reproductive system without any outward signs.
PID may also lead to:
- Increased risk of ectopic pregnancy
- Increased risk of miscarriages and stillbirths
- Higher incidence to premature births and low birth weight in infants
Chlamydia Symptoms In Females
Chlamydia symptoms in females are rare. Roughly 7 in 10 women dont experience any symptoms. The infection may be asymptomatic, meaning that people dont know they have it.
If signs and symptoms occur, they usually happen one to three weeks after the exposure, but could start much later. The symptoms are often mild and passing, and easy to overlook.
Some of the potential signs and symptoms of chlamydia include:
- lower abdominal pain
You May Like: 90 Probationary Period Employment Form
Can You Get Chlamydia If You Use A Condom
A condom lowers your chances of getting chlamydia if used correctly.
Correct use of a condom includes:
Read Also: Using Birth Control To Stop Period Once It Starts
What Are The Pros And Cons Of An Iud
In addition to the advantages previously mentioned, IUDs have long-lasting effects but can be reversed simply by removing the IUD. What makes the IUD appealing to many is that you visit an office once to have it inserted then you dont have to remember on a daily basis to take a pill. It is the most effective but also reversible form of contraception.
The biggest disadvantage of IUDs is the discomfort they can cause women. There are a wide array of side effects that can come along with them including abdominal or pelvic pain, nausea, vomiting, migraines, headaches, spotting or irregular bleeding, and breast tenderness. The side effects vary depending on which type of IUD you get.
This does not typically happen but there is a slim chance your IUD could fall out, most commonly during a period in the first three months. Your OBGYN may recommend that you check to feel for the IUD string occasionally but never pull it out. If your IUD does become dislodged, see your OBGYN ASAP to have it reinserted.
Written by Mid-Atlantic Women’s Care on April 16, 2020. Posted in Blog, Well-Women Care.
You May Like: Dark Brown Discharge Instead Of Period
Tips For Your Pap Smear
- Do not have sex before your pap smear
- Do not use lubricants or lotions in or around the vagina ahead of your pap smear
- Do not douche ahead of your pap smear, health professionals generally recommend that you do not engage in vaginal washing as this can have an impact on the natural flora and fauna balance of the vagina. Read: Bacterial vaginosis vs yeast infection: similarities and differences.
Take a deep breath! Its understandable that you may be feeling nervous ahead of your pap smear, but you are doing the right thing by checking in on your health. Prevention and early diagnosis are truly the best cure.
How Long Does It Take For Gonorrhea To Show Up
It is very common among young adults that are sexually active. This infection is caused by a bacterium that can affect the genitals, mouth or anus. Signs and symptoms are not common but, include painful urination, pus like discharges from the penis and pain/swelling in one testicle for men and, painful urination, intercourse as well as abdominal pain and abnormal vaginal bleeding for women.
Gonorrhea Incubation Period: the incubation period ranges from 1 to 14 days. Men who show symptoms, start noticing them two to five days post exposure. Women, on the other hand, develop them in the first 10 days following infection.
Gonorrhea Window Period: it is between 2 to 6 days.
Also Check: Do Uti Antibiotics Cure Chlamydia
Don’t Miss: Can You Donate Plasma On Your Period
Seven Signs That You Might Have An Std
April is National STD Awareness Month, a perfect time for the medical specialists at PGOMG to educate the public on symptoms that may be caused by sexually transmitted disease , as well as when its necessary to get screened. When should you suspect that your symptoms are related to an STD? There are seven major signs that may indicate that your discomfort is more than just a passing phase.
1. You had unprotected intercourse.
Contraception like the birth control pill or an IUD can prevent pregnancy, but it does not protect against STDs. Proper use of a condom during intercourse is incredibly important in order to prevent contracting an STD.
Do I need to get tested? Yes. Please contact your PGOMG provider immediately and request STD screening.
2. Intercourse is painful.
There are a few reasons why intercourse may be painful, and the presence of an STD is one of them. Intercourse is most often painful or uncomfortable due to gynecological changes, such as vaginal dryness, itching, or burning, all of which are common STD symptoms.
Do I need to get tested? Maybe. Your PGOMG provider can advise on whether STD screening is appropriate. Painful intercourse can be a sign of other underlying medical conditions, so even if you do not suspect an STD, it is still important to contact PGOMG if sex is painful.
3. You have discharge.
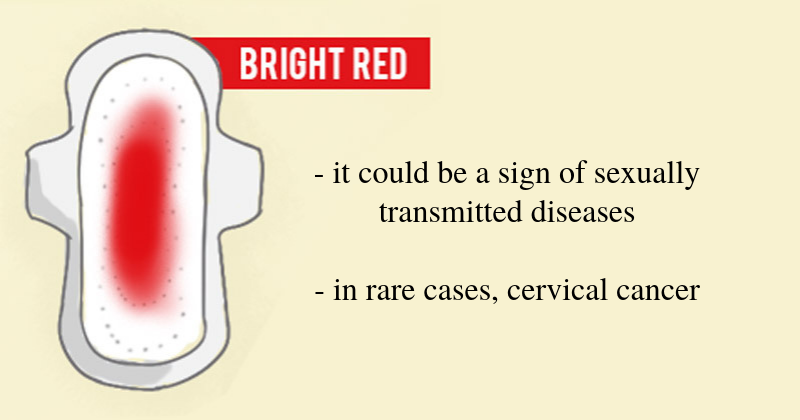
4. You are experiencing spotting.
5. Urinating is painful.
6. You developed a rash or a sore.
7. You are experiencing abnormal uterine bleeding.
Obgyn Myth #: If You Get The Gardasil Shot Or A Similar Vaccine Against Hpv You Dont Need A Pap Smear
The HPV vaccine helps to prevent certain strains of the virus but it does not protect against all strains of the virus and therefore cannot prevent all cases of cervical cancer. It is possible to get HPV despite getting the vaccination. So while getting them is important, vaccines are not always 100% effective.
It is crucial to continue getting screened for cervical cancer even if youve been vaccinated.
Written by Mid-Atlantic Women’s Care on July 21, 2020. Posted in Blog, Well-Women Care.
No matter your relationship status, Sexually Transmitted Infections should be on everyones health radar. STI rates are higher than ever before in the US, and both chlamydia and gonorrhea have the potential of becoming antibiotic-resistant. While there may be stigmas surrounding STIs that need to be banished, it is important that you are knowledgeable about STIs, their prevalence, and how they can affect you. Too few women are seeking out screening for sexually transmitted diseases.
You should not feel ashamed about your sexual activity or STI status, but rather you should take responsibility for your health and safety and that of your sexual partners. The answer to how often you should get tested for STIs may surprise you.
Also Check: 90 Day Employment Probationary Period Template
